WHY CAN'T MY PATIENT SEE WELL WITH SPECIALTY LENSES?
Specialty contact lenses are able to help patients who cannot see clearly with standard contact lenses or glasses. Patients who have abnormalities on the anterior portion of the cornea can benefit from the optics of custom soft, hybrid, or GP lens options. Irregular astigmatism can be treated with a variety of specialty contact lenses, and a patient’s quality of vision can be dramatically improved. But what happens when a patient is fit with a specialty lens and still cannot see well?
What to Do
1. Check anterior and posterior segment ocular health.
Figure 1. A patient who has macular edema, contributing to poor vision.
I’ve had several patients present to the office for a specialty contact lens consultation. Usually, such patients have seen a primary eyecare practitioner for a comprehensive eye exam and then are sent to me for a contact lens fitting. One patient who had keratoconus could see only 20/200 during the diagnostic fitting. I was puzzled as to why I could not get the vision any better, so I performed a few extra tests. Optical coherence tomography of the macula showed macular edema (Figure 1), which was completely unrelated to the patient’s irregular astigmatism. We often assume that vision loss and greatly reduced vision is related to an irregular corneal condition, but sometimes patients have multiple problems within their visual system. Practitioners should thoroughly evaluate the lens, macula, optic nerve, and retina to determine whether the cause of the decreased vision is solely due to the cornea.
2. Do not assume that power changes to existing contact lenses are purely related to the cornea
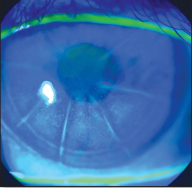
Figure 2. Radial keratotomy scarring incisions inside pupil margins can cause distorted, blurry vision, even with the best specialty lens.
When patients have been wearing specialty lenses for a year or longer, they typically present to your office annually for their comprehensive eye exam. At this visit, be sure to evaluate the contact lenses before removing them, including a careful sphero-cylindrical over-refraction. This can provide great information on not only changes to the contact lenses, but changes to the eye itself. Many times, patients will present with decreased vision, and during the over-refraction, I find a large change in prescription. In such cases, it is helpful to complete a thorough eye health evaluation and note any changes from their last visit. Many times, the power change or decreased vision is due to a cataract that needs to be removed. Sometimes a simple power change of the contact lenses will not do the trick to increase visual acuity.
3. There are posterior cornea limitations.
If patients have irregular astigmatism, a posterior chamber intraocular lens from cataract surgery, and a completely normal retina, you can be pretty confident that vision will improve with a specialty lens. What if you fit them and they have great vision, but complain of shadowing and haloes? If the media of the eye is clear and the contact lens fit is perfect, what could be causing the problem? Check the posterior cornea, if you are able. The posterior cornea can often be to blame for decreased and distorted vision. This is especially true for radial keratotemy patients. When the incisions are extremely deep and/or extend into the center of the pupil, vision can be affected (Figure 2). Most all specialty lenses will not work for these types of patients, and detailed patient education is important.